Calcaneus (Heel Bone) Fractures
Fractures of the heel bone, or calcaneus, can be disabling injuries.
They most often occur during high-energy collisions — such as a fall from height or a motor vehicle crash. Because of this, calcaneus fractures are often severe and may result in long-term problems.
The calcaneus is the most frequently fractured tarsal bone. Tarsal bone fractures account for about 2% of all adult fractures. Of these, 60% are calcaneus fractures.
The heel bone is often injured in a high-energy collision where other parts of the skeleton are also injured. In up to 10% of cases, the patient can also sustain a fracture of the spine, hip, or the other calcaneus.
Injuries to the calcaneus often damage the subtalar joint and cause the joint to become stiff. This makes it difficult to walk on uneven ground or slanted surfaces.
The severity of a fracture usually depends on the amount of force that caused the break. There are many types of calcaneus fractures, including:
Stable fracture. This type of fracture is nondisplaced. The broken ends of the bones meet up correctly and are aligned. In a stable fracture, the bones usually stay in place during healing.
Displaced fracture. When a bone breaks and is displaced, the broken ends are separated and do not line up. This type of fracture often requires surgery to put the pieces back together.
Open fracture. Broken bones that break through the skin are called open, or compound. These types of injuries often involve much more damage to the surrounding muscles, tendons, and ligaments. Open fractures have a higher risk for complications and take a longer time to heal.
Closed fracture. With this injury, the broken bones do not break the skin. Although the skin is not broken, internal soft tissues can still be badly damaged.
Comminuted fracture. This type of break is very unstable. The bone shatters into three or more pieces.
The calcaneus can be injured in a fall, twisting injury, or motor vehicle collision. A simple twisting injury may result in the calcaneus being cracked. The force of a head-on car collision may result in the bone being shattered (comminuted fracture).
Different causes can result in similar fracture patterns. For example, when landing on your feet from a fall, your body's weight is directed downward. It drives the talus bone down into the calcaneus. In a motor vehicle crash, the calcaneus is driven up against the talus. In both cases, the resulting fracture patterns are similar. The greater the impact, the more the calcaneus is damaged.

(Left) In some injuries, the talus is forced downward and acts like a wedge to fracture the calcaneus. (Right) This computerized reconstruction of a calcaneus fracture shows the amount of damage that can occur.
The most common symptoms of a calcaneus fracture are:
- Pain
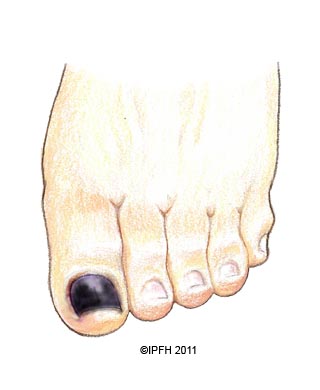
- Bruising
- Swelling
- Heel deformity
- Inability to put weight on the heel or walk
In some minor calcaneus fractures, the pain is not enough to stop you from walking, but you may limp. This is because when you walk, the Achilles tendon acts through the calcaneus to support your body weight. If the calcaneus is deformed following an injury, the muscle and tendon cannot generate enough power to support your weight. Your foot and ankle will feel unstable, and you will walk differently.
It is important that your podiatrist knows the circumstances of your injury. For example, if you fell from a tree, how far did you fall? It is just as important for your podiatrist to know if you have any other injuries or medical problems, such as diabetes. Your podiatrist also needs to know if you take any medications.
After discussing your symptoms and medical history, your podiatrist will do a careful examination. He or she will look for other injuries and for areas where the skin is damaged or punctured. Your podiatrist will check to see if there is a good blood supply to your foot and if the nerves to your foot are working properly. To determine whether you have injured any other areas of your body, your podiatrist will examine the rest of your injured leg, your other leg, your pelvis, and your spine.
Other tests that may help your podiatrist confirm your diagnosis include:
X-rays. This test is the most common and widely available diagnostic imaging technique. X-rays create images of dense structures, like bone, so they are particularly useful in showing fractures.
Computed tomography (CT) scan. After reviewing your x-rays, your podiatrist may recommend a CT scan of your foot. This imaging tool combines x-rays with computer technology to produce a more detailed, cross-sectional image of your body. It can provide your podiatrist with valuable information about the severity of the fracture. Studying CT scans helps your podiatrist plan your treatment. He or she will often show you the images to help you understand the nature and severity of your injury.
- The cause of your injury
- Your overall health
- The severity of your injury
- The extent of soft tissue damage
Because most calcaneus fractures cause the bone to widen, the goal of treatment is to restore the normal anatomy of the heel. In general, patients whose normal heel anatomy is restored have better overall outcomes. Recreating normal anatomy, however, most often involves surgery. Surgery is associated with a higher risk of complications.
Nonsurgical Treatment
If the pieces of broken bone have not been displaced by the force of the injury, you may not need surgery. Casting or some other form of immobilization may be an option. This will keep the broken ends in proper position while they heal.
You will not be able to put any weight on your foot until the bone is completely healed. This may take 6 to 8 weeks, and perhaps longer.
Surgical Treatment
If the bones have shifted out of place (displaced), you may need surgery.
Timing of surgery. If the skin around your fracture has not been broken, your doctor may recommend waiting until swelling has gone down before having surgery. Keeping your leg immobilized and elevated for several days will decrease swelling. It also gives skin that has been stretched a chance to recover. This waiting period before the operation often improves your overall recovery from surgery and decreases your risk of infection.
Open fractures, however, expose the fracture site to the environment. They urgently need to be cleansed and require immediate surgery.
Early surgery is also often recommended for an avulsion fracture. Although uncommon, a piece of the calcaneus can be pulled off when the Achilles tendon tears away from the bone (avulsion). For this type of fracture, early surgery can decrease the risk of injury to the skin around the Achilles tendon.
Surgical procedure. The following procedures are used for various types of calcaneus fractures.
- Open reduction and internal fixation. During this operation, the bone fragments are first repositioned (reduced) into their normal alignment. They are held together with special screws or metal plates and screws.
- Percutaneous screw fixation. Sometimes, if the bone pieces are large, they can be moved back into place by either pushing or pulling on them without making a large incision. Special screws can be placed through small incisions to hold your bone pieces together.

(Left) A displaced fracture of the calcaneus. (Right) The fracture has been reduced and the bones held in place with screws.

The typical method of realigning the bone fragments and holding them in place with metal plates and screws.
Bones have a remarkable capacity to heal. The more severe your injury, however, the longer your recovery may be. Patients with more severe fractures are also more likely to suffer some degree of permanent loss of function, regardless of treatment.
Rehabilitation
Whether you have surgery or not, your rehabilitation will be very similar. How long it takes to return to daily activities varies with different types of fractures. It depends on the severity of the injury. Some patients can begin weight-bearing activities a few weeks after injury or surgery; some patients may need to wait 3 or more months before putting any kind of weight on the heel.
- Early motion. Many podiatrists encourage motion of the foot and ankle early in the recovery period. For example, some patients are instructed to begin moving the affected area as soon as their pain allows. Patients who have had surgery are instructed to begin moving the affected area as soon as the wound heals to the podiatrist's satisfaction.
- Physical therapy. Specific exercises can improve the range of motion in your foot and ankle, and strengthen supporting muscles. Although they are often painful at the beginning and progress may be difficult, exercises are required in order for you to resume normal activities.
- Weight-bearing. When you begin walking, you may need to use a cane and wear a special boot. It is very important to follow your doctor's instructions for walking on your foot. If you place weight on your foot too soon, the bone pieces may move out of place and you might require surgery. If you have had surgery, the screws might loosen or break and the bone may collapse. This may not occur the first time you walk on it, but if the bone is not healed and you continue to walk on your foot, the metal will eventually break.

Six months after surgery, this patient's hardware has failed. Several screws have broken and the calcaneus has collapsed. This patient required major reconstruction, and today walks with a limp and has little motion in the foot.
Complications
There is a range of complications with calcaneus fractures. Minor complications include:
- Small or temporary areas of delayed wound healing
- Nerve irritation around the incision
- Tendon irritation caused by the screws
- Joint stiffness
- Chronic pain
Major complications include:
- Blood clots
- Failure of the wound to heal
- Infection
- Collapse of bone
- Arthritis (with or without surgery)
Smoking affects both bone and skin healing, so it is important to tell your doctor if you smoke. Some surgeons will not perform surgery on a patient who smokes because of the increased risk of serious complications. Even without surgery, your bone may take longer to heal if you smoke.
Additional surgery is usually required in cases of infection or difficult wound healing. If all methods of solving the problem have failed, amputation may be considered.
If your injury is minor, such as a crack in the bone with little muscle damage, you may be able to resume normal activities 3 to 4 months after surgery. If the fracture is severe, however, it may take 1 to 2 years before recovery is complete.
Despite the best efforts of the doctor and patient, normal foot and ankle motion is rarely regained after a severe fracture. A patient who is not very active might tolerate a foot that is not normal. On the other hand, a patient whose job or recreational activities require a lot of walking or climbing will notice limitations much more.
Common Problems
Common problems that may persist after recovery include:
- Skin irritation. Footwear can irritate the skin or tendons in the affected area.
- Altered gait. In some cases, the arch of the foot has not been restored, or the Achilles tendon has not been attached at its normal distance from the ankle. Full subtalar joint motion is rarely regained in these cases, and this changes the way the patient walks. Patients may have problems walking on uneven ground, such as grassy surfaces or hills.
- Pain. If the calcaneus remains deformed, the patient may experience continued ankle pain and limited motion. Even if the heel anatomy is perfectly restored, the patient may still have discomfort. This can happen because of the injured soft tissues or limited range of ankle and subtalar motion. Although relatively uncommon, pain can be caused by irritation from the plates or screws.
Further Treatments
A simple shoe modification may help chronic problems. You may need to wear a heel pad, lift, or shoe cup, as well as special shoes with extra depth in the toe compartment.
Sometimes, another major operation is required. If the bone has healed in a deformed position, or if the subtalar joint becomes arthritic, the joint may need to be fused. The goal of this procedure is to help the talus and the calcaneus grow together and form one bone. Fusion also means that no more motion can occur between the two bones.
If the bone is badly deformed, the surgeon may attempt to correct some or all of the deformity along with fusion of the bones. These surgeries usually require several months for recovery.
Experts are still debating over the best treatment method for calcaneus fractures. As is usually the case, no single method works the same for everyone. Patients whose x-rays show completely normal heel anatomy often still have fracture symptoms after surgery. On the other hand, the calcaneus can look quite deformed on an x-ray, but the patient may have few, if any, symptoms.
There have also been studies that compared results in patients whose fractures were treated with and without surgery. Some studies show a significant benefit of surgery, while other studies show less benefit for certain patients.
As a result, experts continue to work to improve the outcomes of these injuries. Some new developments include:
- Using smaller incisions for reducing and fixing the fracture
- Defining which treatment method works best for which type of fracture
- Defining which treatment method works best for different types of patients; for example, smokers or people with diabetes
- Inventing better plates and screws

 Halloween originated in Ireland over 2,000 years ago
Halloween originated in Ireland over 2,000 years ago