Arthritis of the Foot and Ankle
Although there is no cure for arthritis, there are many treatment options available. It is important to seek help early so that treatment can begin as soon as possible. With treatment, people with arthritis are able to manage pain, stay active, and live fulfilling lives, often without surgery.Arthritis is the leading cause of disability in the United States. It can occur at any age, and literally means "pain within a joint." As a result, arthritis is a term used broadly to refer to a number of different conditions.
There are three types of arthritis that may affect your foot and ankle.
Osteoarthritis
Osteoarthritis, also known as degenerative or "wear and tear" arthritis, is a common problem for many people after they reach middle age. Over the years, the smooth, gliding surface covering the ends of bones (cartilage) becomes worn and frayed. This results in inflammation, swelling, and pain in the joint.
Osteoarthritis progresses slowly and the pain and stiffness it causes worsens over time.Rheumatoid Arthritis
Unlike osteoarthritis which follows a predictable pattern in certain joints, rheumatoid arthritis is a system-wide disease. It is an inflammatory disease where the patient's own immune system attacks and destroys cartilage.
Post-Traumatic Arthritis
Post-traumatic arthritis can develop after an injury to the foot or ankle. This type of arthritis is similar to osteoarthritis and may develop years after a fracture, severe sprain, or ligament injury.
Osteoarthritis
Many factors increase your risk for developing osteoarthritis. Because the ability of cartilage to heal itself decreases as we age, older people are more likely to develop the disease. Other risk factors include obesity and family history of the disease.
Rheumatoid Arthritis
The exact cause of rheumatoid arthritis is not known. Although it is not an inherited disease, researchers believe that some people have genes that make them more susceptible. There is usually a "trigger," such as an infection or environmental factor, which activates the genes. When the body is exposed to this trigger, the immune system begins to produce substances that attack the joint. This is what may lead to the development of rheumatoid arthritis.
Post-Traumatic Arthritis
Fractures - particularly those that damage the joint surface - and dislocations are the most common injuries that lead to this type of arthritis. An injured joint is about seven times more likely to become arthritic, even if the injury is properly treated. In fact, following injury, your body can secrete hormones that stimulate the death of your cartilage cells.
There are 28 bones and more than 30 joints in the foot. Tough bands of tissue, called ligaments, keep the bones and joints in place. If arthritis develops in one or more of these joints, balance and walking may be affected.

Joints and bones of the foot and ankle.
The joints most commonly affected by arthritis in the lower extremity include:
- The ankle (tibiotalar joint). The ankle is where the shinbone (tibia) rests on the uppermost bone of the foot (the talus).
- The three joints of the hindfoot. These three joints include:
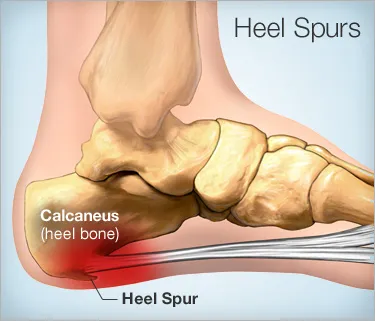
- The subtalar or talocalcaneal joint, where the bottom of the talusconnects to the heel bone (calcaneus);
- The talonavicular joint, where the talus connects to the inner midfoot bone (navicular); and
- The calcaneocuboid joint, where the heel bone connects to the outer midfoot bone (cuboid).
- The midfoot (metatarsocunieform joint). This is where one of the forefoot bones (metatarsals) connects to the smaller midfoot bones (cunieforms).
- The great toe (first metatarsophalangeal joint). This is where the first metatarsal connects to the great toe bone (phalange).This is also the area where bunions usually develop.
Signs and symptoms of arthritis of the foot vary, depending on which joint is affected. Common symptoms include:
- Pain or tenderness
- Stiffness or reduced motion
- Swelling
- Difficulty walking due to any of the above
Your doctor will base a diagnosis using your medical history, symptoms, a physical examination, and additional tests.
Medical History and Examination
A medical history is important to understand more about the problem. Your doctor will want to know when the pain started and when it occurs. Is it worse at night? Does it get worse when walking or running? Is it continuous, or does it come and go?
He or she will want to know if there was a past injury to the foot or ankle. If so, your doctor will discuss your injury, when it occurred, and how it was treated.Your doctor will want to know if the pain is in both feet or only in one foot, and where it is located exactly. Footwear will be examined, and any medications will be noted.
Additional Tests
One of the tests performed during the physical examination is the gait analysis. This shows how the bones in the leg and foot line up with walking, measures stride, and tests the strength of the ankles and feet.
X-rays can show changes in the spacing between bones or in the shape of the bones themselves. Weight-bearing X-rays are the most valuable additional test in diagnosing the severity of arthritis.A bone scan, computed tomographic (CT) scan, or magnetic resonance image (MRI) may also be used in the evaluation.
Depending on the type, location, and severity of the arthritis, there are many types of treatment available.
Nonsurgical Treatment
Nonsurgical treatment options include:
- Pain relievers and anti-inflammatory medications to reduce swelling
- Shoe inserts (orthotics), such as pads or arch supports
- Custom-made shoe, such as a stiff-soled shoe with a rocker bottom
- An ankle-foot orthosis (AFO)
- A brace or a cane
- Physical therapy and exercises
- Weight control or nutritional supplements
- Medications, such as a steroid medication injected into the joint
Surgical Treatment
If arthritis doesn't respond to nonsurgical treatment, surgical treatment might be considered. The choice of surgery will depend on the type of arthritis, the impact of the disease on the joints, and the location of the arthritis. Sometimes more than one type of surgery will be needed.
Surgery performed for arthritis of the foot and ankle include arthroscopic debridement, arthrodesis (or fusion of the joints), and arthroplasty (replacement of the affected joint).Arthroscopic Debridement

A flexible, fiberoptic pencil-sized instrument (arthroscope) is inserted into the joint through a series of small incisions through the skin.
The arthroscope is fitted with a small camera and lighting system, as well as various instruments. The camera projects images of the joint on a television monitor. This enables the surgeon to look directly inside the joint and identify the problem areas.
Small instruments at the end of the arthroscope, such as probes, forceps, knives, and shavers, are used to clean the joint area of foreign tissue, inflamed tissue that lines the joint, and bony outgrowths (spurs).
Arthrodesis or Fusion

(Reproduced with permission from Abdo RV, Iorio LJ: Rheumatoid Arthritis of the Foot and Ankle J Am Acad Orthop Surg 1994;2:326-332.)
The surgeon uses pins, plates and screws, or rods to hold the bones in the proper position while the joint(s) fuse. If the joints do not fuse (nonunion), this hardware may break.
A bone graft is sometimes needed if there is bone loss. The surgeon may use a graft (a piece of bone, taken from one of the lower leg bones or the wing of the pelvis) to replace the missing bone.
This surgery is typically quite successful. A very small percentage of patients have problems with wound healing. These problems can be addressed by bracing or additional surgery.
The biggest long-term problem with fusion is the development of arthritis at the joints adjacent to those fused. This occurs from increased stresses applied to the adjacent joints.
Arthroplasty or Joint Replacement

Although not as common as as total hip or knee joint replacement, advances in implant design have made ankle replacement a feasible option for many people.
In addition to providing pain relief from arthritis, ankle replacements offer patients better mobility and movement compared to fusion. By allowing motion at the formerly arthritic joint, less stress is transferred to the adjacent joints. Less stress results in reduced occurance of adjacent joint arthritis.
Ankle replacement is most often recommended for patients with:
- Advanced arthritis of the ankle
- Destroyed ankle joint surfaces
- An ankle condition that interferes with daily activities
Surgical Recovery
Foot and ankle surgery can be painful. Pain relievers in the hospital and for a time period after being released from the hospital may help.
It is important to keep your foot elevated above the level of your heart for one to two weeks following surgery.Your doctor may recommend physical therapy for several months to help you regain strength in your foot or ankle and to restore range of motion. Ordinary daily activities usually can be resumed in three to four months. You may need special shoes or braces.
In most cases, surgery relieves pain and makes it easier to perform daily activities. Full recovery takes four to nine months, depending on the severity of your condition before surgery, and the complexity of your procedure.

 In Your 20’s: Accidents and injuries are the most common cause of
In Your 20’s: Accidents and injuries are the most common cause of  Our bodies change as we get older. That’s no secret. Men and women alike experience physical, hormonal, and emotional changes as we age. This has an impact on our health and general well-being. One area that has a huge impact on our ability to experience and enjoy the world is our
Our bodies change as we get older. That’s no secret. Men and women alike experience physical, hormonal, and emotional changes as we age. This has an impact on our health and general well-being. One area that has a huge impact on our ability to experience and enjoy the world is our 