What Is Achilles Tendon Inflammation? What Is Achilles Tendinitis?
Achilles tendinitis (tendonitis) or Achilles tendon inflammation occurs when the Achilles tendon becomes inflamed as a result of the Achilles tendon being put under too much strain. The Achilles tendon joins the calf muscles to the heel bone, and is found at the back of a person's lower leg. It is the largest tendon in the body and is able to endure great force, but is still susceptible to injury.
Achiles tendinitis is usually the result of strenuous, high impact exercise, such as running. If ignored, Achilles tendinitis can lead to the tendon tearing or rupturing, and therefore it is important to seek the necessary treatment. Sometimes, treatment can be as simple as getting rest or changing an exercise routine. However, in more severe cases, surgery may be required.
According to Medilexicon's medical dictionary, the Achilles tendon or calcaneal tendon is:
the thick tendon of insertion of the triceps surae (gastrocnemius and soleus) into the tuberosity of the calcaneus.
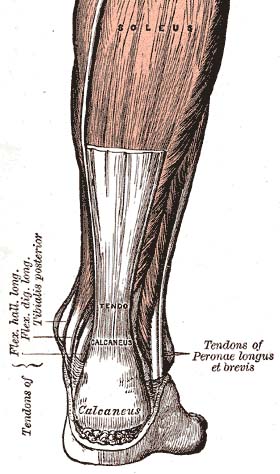
The Achilles tendon (tendo calcaneus) seen from behind
What are the signs and symptoms of Achilles tendinitis?
A symptom is something the patient feels and reports, while a sign is something other people, such as the doctor, detect. For example, pain is a symptom, while a rash is a sign. The most typical symptom of Achilles tendinitis is a gradual buildup of pain that deteriorates with time. Other possible signs and symptoms of Achilles tendinitis are:- the Achilles tendon feels sore a few centimeters above where it meets the heel bone
- lower leg feels stiff
- lower leg feels slow and weak
- slight pain in the back of the leg that appears after running or exercising, and worsens
- pain in the Achilles tendon that occurs while running or a couple of hours afterwards
- greater pain experienced when running fast (such as sprinting), for a long time (such as cross country), or even when climbing stairs
- the Achilles tendon swells or forms a bump
- the Achilles tendon creaks when touched or moved
What are the complications of Achilles tendinitis?
A major complication of Achilles tendinitis is Achilles tendinosis. Achilles tendinosis is a degenerative condition in which the structure of the tendon changes and becomes susceptible to serious damage. This can lead to the tendon tearing and causing great pain.When Achilles tendinosis has occurred, and the tendon has torn, surgery would most likely be performed to repair the tendon damage.
What causes Achilles tendinitis?
There are a number of ways a person can develop Achilles tendinitis. Some causes are easier to avoid than others, but being aware of them can aid earlier diagnosis and help prevent serious injury. Causes of Achilles tendinitis include:- using incorrect or worn out shoes when running/exercising
- not warming up properly before exercise
- increasing intensity of exercise too quickly (e.g. running speed or distance covered)
- prematurely introducing hill running or stair climbing to exercise routine
- running on hard/uneven surfaces
- calf muscle is injured or has little flexibility (this puts a lot of strain on the Achilles tendon)
- sudden intense physical activity such as sprinting for the finish line
How can Achilles tendinitis be prevented?
Although Achilles tendinitis cannot be completely prevented, the risk of developing it can be lowered. Being aware of the possible causes does help, but the risk can be greatly reduced by taking the following precautions:- Getting a variety of exercise - alternating between high-impact exercise (e.g. running) and low-impact exercise (e.g. swimming) can help, as it means there are days when the Achilles tendon is under less tension.
- Limit certain exercises - doing too much hill running, for example, can put excessive strain on the Achilles tendon.
- Wearing the correct shoes and replacing them when worn - making sure they support the arch and protect the heel will create less tension in the tendon.
- Using arch supports inside the shoe - if the shoe is in good condition but doesn't provide the required arch support this is a cheaper (and possibly more effective) alternative to replacing the shoe completely.
- Stretching - doing this before and after exercising helps to keep the Achilles tendon flexible, which means less chance of tendinitis developing. There is no harm in stretching every day (even on days of rest), as this will only further improve flexibility.
- Gradually increasing intensity of workout - Achilles tendinitis can occur when the tendon is suddenly put under too much strain, warming up and increasing the level of activity gradually gives your muscles time to loosen up and puts less pressure on the tendon.
How is Achilles tendinitis diagnosed?
When diagnosing Achilles tendinitis, a doctor will ask the patient a few questions about their symptoms and then perform a physical examination. To perform a physical exam on the Achilles tendon, the doctor will lightly touch around the back of the ankle and tendon to locate the source of the pain or inflammation. They will also test the foot and ankle to see if their range of motion and flexibility has been impaired.The doctor might also order an imaging test to be done on the tendon. This will aid in elimination of other possible causes of pain and swelling, and may help the doctor asses the level of damage (if any) that has been done to the tendon.
Types of imaging tests that could be used for diagnosing Achilles tendinitis are:
- MRI (Magnetic resonance imaging)
- X-ray
- Ultrasound
How can Achilles tendinitis be treated?
The aim when treating Achilles tendinitis is to relieve pain and reduce swelling. The kind of treatment used can vary, based on severity of the condition and whether or not the patient is a professional athlete. After diagnosis, a doctor will decide which method of treatment is required for the patient to undergo, it is likely that they will suggest a combination. Methods used to treat Achilles tendinitis include:- Ice packs - applying these to the tendon, when in pain or after exercising, can alleviate the pain and inflammation.
- Resting - this gives the tissue time to heal. The type of rest needed depends on the severity of the symptoms. In mild cases of Achilles tendinitis, it may mean just reducing the intensity of a workout, in severe cases it might mean complete rest for days or weeks.
- Elevating the foot - swelling can be reduced if the foot is kept raised above the level of the heart.
- Exercise and stretching - a doctor might show the patient some stretching exercises that help the Achilles tendon heal, as well as preventing future injury. They may, instead, refer the patient to a physiotherapist or another specialist. The exercises learned will improve flexibility of the area and likely increase calf strength.
- Pain relievers - non-steroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen can reduce pain and swelling. If you suffer from asthma, kidney disease or liver disease do not take NSAIDs without first checking with your doctor.
- Steroid injections - these can reduce tendon swelling, but should be performed with caution, as this process has been associated with a greater risk of tendon rupture. A doctor would likely perform the injection while scanning the area with ultrasound to reduce this risk.
- Compression bandages and orthotic devices - such as ankle supports and shoe inserts can aid recovery, as they take stress off the Achilles tendon.
- Surgery - as mentioned earlier, surgery is performed to repair any damage to the tendon in cases of Achilles tendinosis. It might also be required if the patient has had recurring Achilles tendinitis and the ongoing inflammation has caused the tendon to rupture. A doctor may also resort to surgery when several of the above treatment methods have proved unsuccessful.
